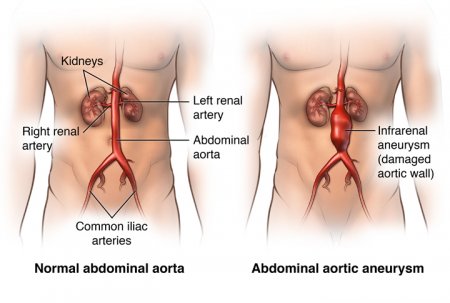
Abdominal aortic aneurysm
- Category: Diseases of the blood vessels
- Views: 46768
An abdominal aortic aneurysm is an enlarged area in the lower part of the aorta, the major blood vessel that supplies blood to the body. The aorta, about the thickness of a garden hose, runs from your heart through the center of your chest and abdomen.
Because the aorta is the body's main supplier of blood, a ruptured abdominal aortic aneurysm can cause life-threatening bleeding.
Depending on the size and the rate at which your abdominal aortic aneurysm is growing, treatment may vary from watchful waiting to emergency surgery.
Once an abdominal aortic aneurysm is found, doctors will closely monitor it so that surgery can be planned if it's necessary. Emergency surgery for a ruptured abdominal aortic aneurysm can be risky.
Hepatitis G
- Category: Gastroenterology
- Views: 48161
Hepatitis G is a newly discovered form of liver inflammation caused by hepatitis G virus (HGV), a distant relative of the hepatitis C virus.
HGV, also called hepatitis GB virus, was first described early in 1996. Little is known about the frequency of HGV infection, the nature of the illness, or how to prevent it. What is known is that transfused blood containing HGV has caused some cases of hepatitis. For this reason, patients with hemophilia and other bleeding conditions who require large amounts of blood or blood products are at risk of hepatitis G. HGV has been identified in between 1-2% of blood donors in the United States. Also at risk are patients with kidney disease who have blood exchange by hemodialysis, and those who inject drugs into their veins. It is possible that an infected mother can pass on the virus to her newborn infant. Sexual transmission also is a possibility.
Often patients with hepatitis G are infected at the same time by the hepatitis B or C virus, or both. In about three of every thousand patients with acute viral hepatitis, HGV is the only virus present. There is some indication that patients with hepatitis G may continue to carry the virus in their blood for many years, and so might be a source of infection in others.
Hepatitis E
- Category: Gastroenterology
- Views: 44101
Hepatitis E is an illness of the liver caused by hepatitis E virus (HEV), a virus which can infect both animals and humans.
HEV infection usually produces a mild disease, hepatitis E. However, disease symptoms can vary from no apparent symptoms to liver failure. In rare cases it can prove fatal, particularly in pregnant women.
Normally the virus infection will clear by itself. However, it has been shown that in individuals with suppressed immune systems, the virus can result in a persistent infection which in turn can cause chronic inflammation of the liver.
Hepatitis D
- Category: Gastroenterology
- Views: 47759
Hepatitis D, also known as the delta virus, is an infection that causes the liver to become inflamed. This swelling can impair liver function and cause long-term liver problems, including liver scarring and cancer. The condition is caused by the hepatitis D virus (HDV). This virus is rare in the United States, but it’s fairly common in the following regions:
- South America
- West Africa
- Russia
- Pacific islands
- Central Asia
- the Mediterranean
HDV is one of many forms of hepatitis. Other types include:
- hepatitis A, which is transmitted through direct contact with feces or indirect fecal contamination of food or water
- hepatitis B, which is spread through exposure to body fluids, including blood, urine, and semen
- hepatitis C, which is spread by exposure to contaminated blood or needles
- hepatitis E, which is a short-term and self-resolving version of hepatitis transmitted through indirect fecal contamination of food or water
Unlike the other forms, hepatitis D can’t be contracted on its own. It can only develop in people who are already infected with hepatitis B.
Hepatitis D can be acute or chronic. Acute hepatitis D occurs suddenly and typically causes more severe symptoms. It may go away on its own. If the infection lasts for six months of longer, the condition is known as chronic hepatitis D. The long-term version of the infection develops gradually over time. The virus might be present in the body for several months before symptoms occur. As chronic hepatitis D progresses, the chances of complications increase. Many people with the condition eventually develop cirrhosis, or severe scarring of the liver.
There’s currently no cure or vaccine for hepatitis D, but it can be prevented in people who aren’t already infected with hepatitis B. Treatment may also help prevent liver failure when the condition is detected early.
Hepatitis C
- Category: Gastroenterology
- Views: 45052
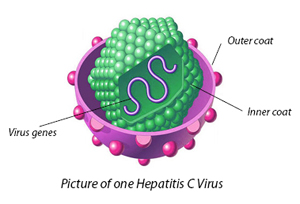
Hepatitis C is a viral infection that causes liver inflammation, sometimes leading to serious liver damage. The hepatitis C virus (HCV) spreads through contaminated blood.
Until recently, hepatitis C treatment required weekly injections and oral medications that many HCV-infected people couldn't take because of other health problems or unacceptable side effects.
That's changing. Today, chronic HCV is usually curable with oral medications taken every day for two to six months. Still, about half of people with HCV don't know they're infected, mainly because they have no symptoms, which can take decades to appear. For that reason, the U.S. Centers for Disease Control and Prevention recommends a one-time screening blood test for everyone at increased risk of the infection. The largest group at risk includes everyone born between 1945 and 1965 — a population five times more likely to be infected than those born in other years.
Hepatitis B
- Category: Gastroenterology
- Views: 44814

Hepatitis B is a serious liver infection caused by the hepatitis B virus (HBV). For some people, hepatitis B infection becomes chronic, meaning it lasts more than six months. Having chronic hepatitis B increases your risk of developing liver failure, liver cancer or cirrhosis — a condition that causes permanent scarring of the liver.
Most people infected with hepatitis B as adults recover fully, even if their signs and symptoms are severe. Infants and children are more likely to develop a chronic hepatitis B infection. A vaccine can prevent hepatitis B, but there's no cure if you have it. If you're infected, taking certain precautions can help prevent spreading HBV to others.
Hepatitis A
- Category: Gastroenterology
- Views: 45656
Hepatitis A is a highly contagious liver infection caused by the hepatitis A virus. The virus is one of several types of hepatitis viruses that cause inflammation and affect your liver's ability to function.
You're most likely to contract hepatitis A from contaminated food or water or from close contact with someone who's infected. Mild cases of hepatitis A don't require treatment, and most people who are infected recover completely with no permanent liver damage.
Practicing good hygiene, including washing hands frequently, is one of the best ways to protect against hepatitis A. Vaccines are available for people most at risk.
Gallstones and Bile Duct Stones
- Category: Gastroenterology
- Views: 45412
Gallstones, which are created in the gallbladder, form when substances in the bile create hard, crystal-like particles. Cholesterol stones, as the name implies, are made of cholesterol and appear light in color. Eighty percent of gallstones are formed this way.
Pigment stones are small, dark stones made of bilirubin and calcium salts that are found in bile. About twenty percent of gallstones are pigment stones. Risk factors for pigment stones include:
- cirrhosis of the liver
- biliary tract infections
- hereditary blood cell disorders (such as sickle cell anemia)
Gallstones can be as small as a grain of salt or as large as a golf ball. The gallbladder may develop many smaller stones, or a single, often large one. It may even develop several thousand stones.
Chronic Pancreatitis
- Category: Gastroenterology
- Views: 44045
Chronic pancreatitis is different from acute pancreatitis in that the inflammation and damage develop more slowly, and can become increasingly bad over time. The pancreas becomes scarred and loses its ability to make enough digestive enzymes and insulin. Thickening of the pancreatic juices may result in clogging of the pancreatic ducts and pancreatic stones which, along with damage to the ducts themselves can result in aggravation of the pancreatitis due to obstruction.
When chronic pancreatitis occurs in many members of the family, sometimes starting with childhood attacks, it is called familial pancreatitis. A similar form of chronic pancreatitis occurs in tropical countries, often associated with severe malnutrition.
Cholecystitis
- Category: Gastroenterology
- Views: 43326

Cholecystitis refers to inflammation of the gallbladder. Cholecystitis may be either acute or chronic. Acute cholecystitis results from blockage of the outlet of the gallbladder, usually by a gallstone. This leads to a build up of concentrated bile in the gallbladder that may become infected. Many patients with cholecystitis complain of abdominal pain in the upper-right quadrant which usually commences after a meal and can last from minutes to days, but which usually lasts for less than 24 hours. This pain often passes into the back and up to the right shoulder blade.
Other symptoms include fever, chills, nausea and vomiting. The abdomen may be very tender to touch beneath the right ribs. Patients with these symptoms should see their doctor whom may order blood tests, an abdominal ultrasound or possibly a CT scan of the abdomen. The usual treatment for attacks of acute cholecystitis is removal of the gallbladder (cholecystectomy), usually by laparoscopic surgery.